Social Anxiety Disorder & Substance Abuse in a Dual Diagnosis
Individuals with Social Anxiety Disorder (SAD) often turn to other substances to manage their symptoms, leading to potential abuse and dependency. It’s vital for families to recognize this disorder as a legitimate mental health condition that requires professional treatment.
Social Anxiety Disorder (Social Phobia): A DSM-5 Overview
Social Anxiety Disorder (SAD), also known as Social Phobia, is detailed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) as a significant and chronic mental health condition.
It is characterized by an intense fear or anxiety about social situations where the individual is exposed to possible scrutiny by others. This fear often centers on worries about being judged negatively, feeling embarrassed, or being rejected in social or performance-related situations.

Diagnostic Criteria from the DSM-5 for SAD
To be diagnosed with Social Anxiety Disorder according to the DSM-5, an individual must meet specific criteria:
Marked Fear or Anxiety
The person experiences significant fear or anxiety about one or more social situations where they are exposed to possible scrutiny by others. Common examples include social interactions (e.g., having a conversation), being observed (e.g., eating or drinking), and performing in front of others (e.g., giving a speech).
Avoidance or Endured with Intense Fear
Social situations almost always provoke fear or anxiety, and they are either avoided or endured with intense fear or anxiety. Out of Proportion: The fear or anxiety is disproportionate to the actual threat posed by the social situation and to the sociocultural context.
Out of Proportion
The fear or anxiety is disproportionate to the actual threat posed by the social situation and to the sociocultural context.
Persistence
The fear, anxiety, or avoidance is persistent, typically lasting for six months or more.
Significant Distress or Impairment
The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Not Attributable to Other Factors
The fear, anxiety, or avoidance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition. It is also not better explained by another mental disorder.
Features and Symptoms of Social Anxiety Disorder
Individuals with Social Anxiety Disorder may exhibit a range of behaviors and physical symptoms in response to feared social situations, including:
- Avoid eye contact, social interactions, or situations where they might be the center of attention.
- Physical symptoms of anxiety such as blushing, sweating, trembling, nausea, or difficulty speaking.
- Excessive worry about upcoming social situations, often for days or weeks in advance.
- Low self-esteem and high sensitivity to criticism.
- Difficulty forming and maintaining close relationships.
Differentiation from Other Anxiety Disorders
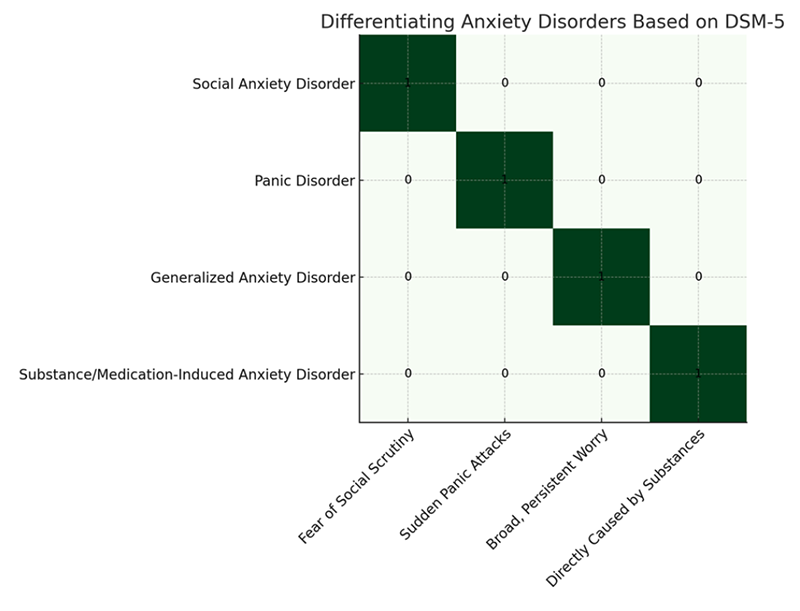
The graph visually differentiates Social Anxiety Disorder (Social Phobia) from Panic Disorder, Generalized Anxiety Disorder (GAD), and Substance/Medication-Induced Anxiety Disorder based on DSM-5 explanations. Each disorder is uniquely characterized by specific criteria:
- Social Anxiety Disorder is marked by a fear of social scrutiny
- Panic Disorder by sudden panic attacks,
Generalized Anxiety Disorder by broad, persistent worry - Substance/Medication-Induced Anxiety Disorder by anxiety directly caused by substances.
This differentiation helps in understanding the distinct nature of these anxiety-related disorders.
Separating Fact from Fiction: Understanding Social Anxiety Disorder
Social Anxiety Disorder (SAD), often misunderstood, is surrounded by myths that can hinder recognition and treatment. Dispelling these myths with facts is crucial for a better understanding and supporting those affected.

Myth 1: SAD is just shyness
- The Truth: While shyness is a common trait, SAD is a recognized mental health condition that significantly impacts daily functioning. Unlike shyness, SAD involves intense fear, anxiety, and avoidance of social situations due to worries about being judged or embarrassed.

Myth 2: People with SAD don’t want to socialize
- The Truth: Individuals with SAD often desire to connect with others but are held back by their fear of social interaction. Their avoidance is not a preference but a coping mechanism to prevent anxiety.

Myth 3: SAD isn’t a serious condition
- The Truth: SAD is a severe and debilitating disorder that can severely affect a person’s quality of life, including their ability to work, attend school, and maintain relationships. It requires professional treatment to manage effectively.
Risky Relief: Understanding Substance Abuse in SAD
The intersection of Social Anxiety Disorder (SAD) and substance abuse disorders is notably complicated by the prescribed medications for anxiety, particularly benzodiazepines. These medications carry significant risks of dependency and addiction, particularly concerning individuals with SAD who may be more susceptible to substance use disorders.
Commonly Prescribed Addictive Medications
Benzodiazepines: Drugs such as Alprazolam (Xanax), Lorazepam (Ativan), Diazepam (Valium), and Clonazepam (Klonopin) are often prescribed for their fast-acting anxiolytic effects. Despite their efficacy in acute scenarios, their potential for addiction and dependency makes them a double-edged sword for individuals with anxiety disorders.
Dangers of Dependency and Exacerbation of SAD
Dependency Risks: The ease with which individuals can develop a physical and psychological dependence on benzodiazepines is alarmingly high. This dependency can quickly escalate from therapeutic use to substance abuse, complicating the treatment of SAD.
Withdrawal and Anxiety Rebound: Discontinuation or reduction in the use of these medications can lead to withdrawal symptoms, which, paradoxically, can include heightened anxiety—potentially worsening the very symptoms they were prescribed to manage.
Long-Term Ineffectiveness: Over time, the body can build tolerance to benzodiazepines, necessitating higher doses to achieve the same anxiolytic effect, further increasing the risk of dependency and addiction.
Alternative Treatment Necessity: Given these risks, there’s a pressing need for alternative treatments that do not carry the same potential for abuse. Psychotherapeutic interventions, like cognitive-behavioral therapy (CBT) and SSRIs, which have a lower risk of addiction, are crucial components of a comprehensive treatment plan for SAD.
The emphasis on the dangers associated with benzodiazepines highlights the complex challenge of treating anxiety disorders like SAD without exacerbating potential substance use problems. This underscores the importance of cautious prescription practices, close monitoring of medication use, and the integration of non-pharmacological treatments to ensure a balanced and safe approach to managing anxiety.
Alcohol, Cannabis, and Nicotine: The Triple Threat in SAD Management
Individuals with Social Anxiety Disorder (SAD) often turn to other substances to manage their symptoms, leading to potential abuse and dependency:
- Alcohol:
- Used for its immediate relaxing and anxiety-reducing effects.
- Facilitates more accessible social interactions but risks dependency.
- Cannabis:
- Sought for its calming effects on anxiety.
- Perceived as a stress reliever, yet poses risks of increased anxiety over time.
- Nicotine:
- Utilized to manage stress and anxiety levels.
- Despite temporary relief, it carries significant health risks and potential for addiction.
These substances, while providing temporary relief, can lead to long-term health issues and complicate the treatment of SAD.

Cognitive-Behavioral Approaches to Social Anxiety: Expert Insights and Strategies
Each book provides strategies and insights for managing and overcoming Social Anxiety Disorder, catering to different preferences for self-help approaches.
"The Shyness and Social Anxiety Workbook: Proven Techniques for Overcoming Your Fears"
by Martin M. Antony and Richard P. Swinson
This workbook offers readers a comprehensive guide to understanding and overcoming social anxiety through cognitive-behavioral therapy techniques. It includes practical exercises and tools to build social skills and reduce social anxiety.
"Overcoming Social Anxiety and Shyness: A Self-Help Guide Using Cognitive Behavioral Techniques"
by Gillian Butler
Gillian Butler’s book provides a step-by-step program based on cognitive-behavioral therapy (CBT) to help readers understand their social anxiety, challenge negative thoughts, and improve confidence in social situations.
"Dying of Embarrassment: Help for Social Anxiety and Phobia"
by Barbara G. Markway, Gregory P. Markway, Cheryl N. Carmin, and C. Alec Pollard
This book offers insight into the lives of individuals suffering from social anxiety disorder. It provides practical advice, based on scientifically backed methods, for overcoming intense fear of social and performance situations.
Final Thought on Social Anxiety Disorder
Our Words for Families Considering Long-Term Treatment
The intersection of Social Anxiety Disorder (SAD) and substance abuse, especially with benzodiazepines, underscores a critical treatment challenge. These medications, while effective, pose significant risks of dependency, complicating SAD’s management. Emphasizing safer, non-addictive treatment options like cognitive-behavioral therapy is essential for a balanced, practical approach to overcoming SAD and its complexities.





