Amongst the career professionals that undergo long-term treatment for chronic addiction, I’ve encountered a group that often goes unnoticed: healthcare professionals. It’s a topic that deserves more attention, not just for the well-being of these individuals, but for the safety of their patients as well.
It’s not unusual for us to treat career professionals from all walks of life at Burning Tree Ranch, but families are often surprised how common it is for us to work with doctors and nurses.
What is it about the professionals that work in the healthcare industry that makes them more prone to substance abuse and chronic relapse? There are a few factors that I can share from my experience and perspective.
Healthcare & Addiction is a Hidden Epidemic
The numbers are sobering. Studies indicate that 10-15% of healthcare workers may struggle with substance abuse at some point in their careers. This statistic hit home for me when I realized it meant that in a typical hospital, several of the professionals we trust with our lives might be silently fighting their own battles.
It turns out that doctors and nurses are people that have their own struggles just like everyone else.
You might think that working in the healthcare field would mean these individuals are more attuned to the physical and mental health consequences of substance use, and perhaps that’s true. But these people also operate in a high-stress environment where success is the only option their patients care about.
When you’re the one tasked with helping the sick, where do you turn for your own healing?
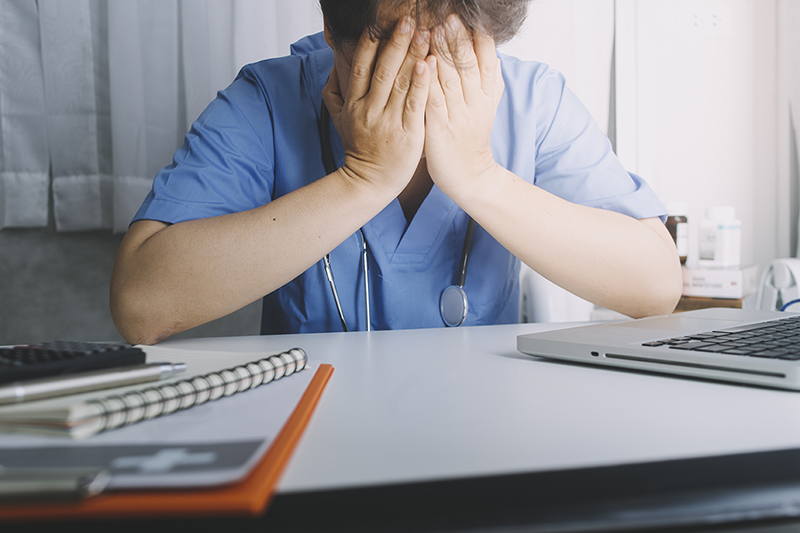
The Constant Pressure Faced by Medical Professionals
Healthcare professionals face a perfect storm of risk factors that can push even the most resilient individuals towards substance abuse. It’s a combination of environmental, psychological, and situational factors that create a uniquely challenging landscape:
- High-stress environments: Medical settings are inherently high-pressure, with decisions that directly impact people’s lives. This constant state of alertness can lead to chronic stress.
- Easy access to prescription medications: The proximity to powerful drugs presents a temptation not present in most other professions, making it dangerously simple to start self-medicating.
- Long, grueling hours: With residents working 80-hour weeks and nurses pulling double shifts, the medical field is notorious for demanding schedules that can lead to burnout and impaired judgment.
- Intense pressure to perform flawlessly: In healthcare, mistakes can be fatal, creating an environment where perfection isn’t just encouraged – it’s expected.
I once spoke with a surgeon who described this constant tension: “It’s like walking a tightrope every day,” he said. “Sometimes, you look for anything to steady your nerves.” This pressure, combined with a culture that often glorifies self-sacrifice and stoicism, can make it difficult for healthcare professionals to admit when they’re struggling and need help.
When you put all of these factors together, you get an individual that is under constant, intense stress combined with an increased exposure and easier access to substances of abuse.
It’s vital for the rest of us as coworkers, patients, and families recognize that despite their training and expertise, medical professionals are human beings vulnerable to the same struggles as anyone else – perhaps even more so due to their unique circumstances.

Increased Exposure & Access to Substances of Abuse
In medical settings, healthcare professionals find themselves in a unique position when it comes to substance abuse. Their work environment provides increased exposure and access to a variety of potent medications.
The most frequently abused substances in these settings are opioids and painkillers, benzodiazepines, and alcohol.
Opioids, including drugs like fentanyl and oxycodone, are particularly problematic due to their high potency and addictive potential.
Benzodiazepines, often prescribed for anxiety or sleep disorders, can become a crutch for stressed medical professionals.
Alcohol, while not unique to healthcare settings, remains a common substance of abuse, often used to unwind after high-stress shifts.
The choice of substance often relates directly to availability and familiarity. A nurse I worked with started her descent into addiction with leftover fentanyl from patients, reasoning that it would otherwise be wasted. She considered it to be a victimless crime.
This kind of rationalization is not uncommon. Many healthcare professionals begin by self-medicating for stress, pain, or sleep issues, using drugs they’re accustomed to handling professionally.
The ease of access combined with intimate knowledge of these substances can create a false sense of security, leading to a slippery slope of misuse. It’s a stark reminder that even those with extensive medical training are not immune to the powerful grip of addiction, and that the very tools used to heal patients can become sources of personal destruction.
What it Looks Like: Signs of Addiction in Healthcare Professionals
Healthcare professionals are highly knowledgeable about the regulations around controlled substances, and they can be quite adept at hiding their struggles. However, over time there may be a mounting pile of evidence hinting at substance abuse, either through their work performance, behavioral patterns, or in related medication documentation.
Changes in Work Performance
- Frequent tardiness or absences
- Errors in documentation or medication administration
- Volunteering for extra shifts, especially nights
Behavioral and Physical Indicators
- Mood swings or irritability
- Isolation from colleagues
- Physical signs like bloodshot eyes or unexplained weight loss
Medication Discrepancies & Clerical Errors
- Higher than average medication waste
- Patients reporting inadequate pain management
- Frequent reports of lost medications

The Far-Reaching Consequences of Unchecked Substance Abuse
When addiction takes hold of a healthcare professional, the ripple effects can be devastating, extending far beyond the individual to impact patients, institutions, and the broader medical community. The consequences are multifaceted and often severe.
Patient Safety
Perhaps the most critical concern is the potential for harm to patients. Impaired judgment, slowed reflexes, and compromised decision-making can lead to medical errors with dire consequences. A surgeon operating under the influence might make a fatal mistake, or a nurse battling addiction might administer incorrect medication dosages. These errors not only jeopardize patient lives but also erode the trust that forms the foundation of healthcare.
Legal and Licensing Issues
Substance abuse often results in license suspension or revocation, effectively ending a medical career that took years of dedication to build. Healthcare professionals may face legal repercussions, including malpractice lawsuits, criminal charges for drug diversion, or DUI offenses. These legal battles can be financially and emotionally draining, further complicating the path to recovery.
Career Setbacks
Even if a healthcare professional manages to retain their license, rebuilding a medical career after addiction is an uphill battle. The stigma associated with substance abuse can make it challenging to find employment, regain hospital privileges, or restore professional relationships. Many find themselves starting over in new specialties or leaving medicine altogether, a significant loss of expertise for the healthcare system.
Personal Life
The toll on personal relationships and finances is often dramatic. Addiction can strain marriages, alienate children, and destroy friendships. The financial impact can be severe, with the high costs of addiction compounded by potential job loss, legal fees, and treatment expenses. Many healthcare professionals find themselves facing bankruptcy or losing homes and savings they’ve worked years to accumulate.
These far-reaching consequences highlight the need to bring more awareness around substance abuse for healthcare professionals. Jeopardizing one’s own health and career is one thing, but in healthcare facilities we also need to think about the safety and health of patients, and the overall integrity of the healthcare system.

Fears & Barriers to Seeking Help
Healthcare professionals battling addiction face a unique set of obstacles when it comes to seeking treatment. These barriers are often deeply rooted in the culture of medicine and the high stakes of their profession, creating a complex web of fears and concerns that can keep them trapped in the cycle of addiction.
Fear of Losing Their License
For many healthcare professionals, their medical license isn’t just a credential—it’s their identity and livelihood. The threat of career destruction looms large over any consideration of seeking help. This fear can be paralyzing, causing many to suffer in silence rather than risk exposure. State medical boards, while increasingly recognizing addiction as a treatable disease, still have the power to suspend or revoke licenses, adding to this fear.
Professional Stigma
There’s often a culture of silence around addiction in medical circles. The expectation of perfection and infallibility in healthcare can make it incredibly difficult for professionals to admit they’re struggling. Colleagues may view addiction as a moral failing rather than a disease, leading to isolation and shame for those affected. This stigma can be particularly pronounced in specialties where substance abuse is seen as especially egregious, such as anesthesiology or emergency medicine.
Denial and Self-Treatment
Medical knowledge can foster a dangerous false sense of control. Healthcare professionals might believe they can manage their substance use because they understand the pharmacology and physiology involved. This can lead to rationalization and attempts at self-treatment, which almost invariably fail and often worsen the problem. The ability to self-prescribe or divert medications can further enable this behavior.
Confidentiality Concerns
In a field where reputation is everything, worrying about damaging one’s professional standing prevents many from seeking help. The fear that colleagues, patients, or employers might discover their struggle can be overwhelming. Even with confidential treatment options available, the tight-knit nature of many medical communities can make healthcare professionals feel exposed and vulnerable.
These barriers can intersect with one another, creating formidable obstacles to seeking recovery at all.
An anesthesiologist I worked with put it bluntly: “I knew I needed help, but I convinced myself I could handle it. The thought of losing everything I’d worked for was paralyzing.” This sentiment is echoed by many healthcare professionals grappling with addiction.
As a whole, the medical community is beginning to recognize the need to address these concerns. Some states have implemented confidential treatment programs specifically for healthcare professionals, designed to provide help while protecting careers.
However, overcoming the deeply ingrained fears and stigmas remains a significant challenge. It’s crucial for healthcare institutions and treatment providers to foster an environment where seeking help for addiction is seen not as a career-ending admission of weakness, but as a responsible step towards better patient care and personal health.

How Can Colleagues & Employers Help?
Adequately addressing a substance abuse issue among healthcare professionals requires a concerted effort from several angles. Colleagues and employers both play a role in creating an environment that prevents substance abuse and supports those struggling with addiction.
First and foremost, it’s important to recognize and report signs of substance abuse. This can be challenging in a culture that often values self-reliance and stoicism, but speaking up could literally save careers and lives. Colleagues should be educated on the signs of impairment and substance abuse, and institutions should have clear, non-punitive reporting protocols in place.
Second, we can foster a workplace culture that encourages and accepts medical professionals to seek help. Employers can implement wellness programs, provide confidential counseling services, and offer education about stress management and the risks of substance abuse. If we can shift the narrative from one of shame and consequence to one of health and recovery, then we’re already taking the first steps towards healing.
Balancing safety and support is perhaps the most delicate aspect of addressing this issue. While patient safety must always be the top priority, we have to remember that healthcare professionals are also people in need of compassionate care.
Employers should have systems in place to immediately remove impaired professionals from patient care while simultaneously connecting them with treatment resources. This might involve temporary reassignment to non-clinical duties or paid leave for treatment. Implementing fair return-to-work policies that include monitoring and support can help professionals recover while eventually regaining their full professional status.

How We Treat Healthcare Professionals in Long-Term Treatment
Doctors, surgeons, nurses, and clerical staff – they all play an important role in serving and healing our communities. Taking the time to regain control of your life is far from an admission of defeat – it’s a significant step towards personal and professional growth.
At Burning Tree Ranch, we use a progress-based approach in a long-term residential treatment setting. We help provide a solid framework for personal growth that fosters a commitment to individual recovery efforts.
Some of the doctors we have treated have expressed gratitude after the Burning Tree Ranch program, claiming it has not only saved their careers, but has given them a better understanding of their patient’s struggles.
There’s very little room in the healthcare industry to forgo treating a complex addiction. It’s an issue that needs to be addressed head-on with an integrative approach that comprehensively treats the physical and mental health of the professionals who themselves have dedicated their lives to healing others.
If this sounds like you or somebody you know, I encourage you to reach out to us for guidance. Our admissions team will help provide a clear path towards recovery, including resources for both employers and families.
Until next time,
Brook